The Plug-and-Play Myth:
What You Were Promised vs. What You Got
If you’re building a health product, you’ve probably been told some version of this:

And yet—despite checking all the boxes—your team hits walls.
Data doesn’t flow. Pilots get delayed. “Compliant” systems don’t work together.
It’s frustrating, confusing, and costly.
So what’s really going on?
This article breaks down why EHR interoperability is so hard in practice, even when the technology should work—and how health startups can avoid the traps, even if you’re not a backend expert.
Why Now: Interop Isn’t Optional Anymore
New regulations like the 21st Century Cures Act are accelerating the demand for data access and exchange. And as decentralized trials and digital health tools expand, “talking to the system” isn’t a nice-to-have—it’s a survival skill.
If your product can’t interoperate with the health ecosystem—from EHRs to labs to payers—you’ll struggle to:
- Land pilots
- Pass compliance reviews
- Scale across multiple sites
- Gain investor or partner trust
The short version?
If your product doesn’t connect, it doesn’t compete.
The Real Problem: Standards ≠ Standardization
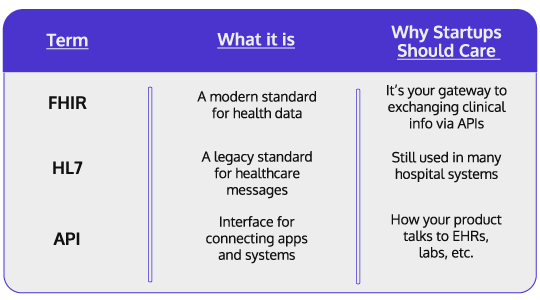
Health tech is full of technical terms that sound like they solve the problem: FHIR. HL7. SMART on FHIR. APIs.
Here’s the catch:
These are standards.
But they’re not standardized in practice.
Let’s break it down:
Sounds great—until you realize:
- One EHR might expose 8 FHIR endpoints, another only 3
- Field names may differ across systems
- “FHIR-compatible” doesn’t mean “plug-and-play”
- Some systems use custom rules that break your assumptions
The result?
Endless engineering cycles untangling field mappings
Bugs and unexpected data failures in production
Delayed pilots and stalled partner integrations
Compliance reviews that fail due to mismatched setups
Multiply that across systems or clinical sites, and you’re not scaling—you’re stuck.
Why Interoperability Really Matters to Startup Teams
You don’t need to be technical to feel the cost:

Pilots fall apart when integrations don’t work

Trials slow down waiting for data access

Enterprise deals vanish if infra can’t scale

Investors hesitate if you can’t prove you’re production-ready
And most of the time, this isn’t a product problem.
It’s an infrastructure problem—caused by trying to DIY what should’ve been baked in.
What Smart Teams Are Doing Differently
Founders who are scaling past these hurdles aren’t building from scratch. They’re:
Choosing tech partners who live and breathe FHIR—not just claim it
Testing in real-world conditions (not just vendor sandboxes)
Automating security, logging, and compliance early
Building with infrastructure that can pass audits, not just demos
Avoiding brittle, self-hosted setups that break under pressure
How Alternova Helps
We’ve seen this story play out over and over—brilliant product teams getting blocked by the messy, underfunded part of the stack: the part that’s supposed to just work.
That’s why we built our EHR hosting platform specifically for health startups and research teams who can’t afford to get stuck:
- Medplum-native, fully managed infrastructure
- SOC2-compliant, HIPAA-ready, audit-tested
- Used in real-world integrations, not just theoretical ones
- Support from engineers who actually know what you’re building
We make FHIR work like it’s supposed to—so your product doesn’t have to fight your platform.
TL; DR
Plug-and-play is still a myth in health tech.
Because “compliant” isn’t the same as usable, scalable, or safe.
If you’re building a health product that needs to connect across systems,
your infrastructure matters more than you think.
Curious how we help health startups launch faster
with real FHIR interoperability, done right?